Understanding bone tumors
Bone tumors can affect any bone in the body and develop in any part of the bone—from the surface to the center of the bone, called the bone marrow. A growing bone tumor—even a benign tumor—destroys healthy tissue and weakens bone, making it more vulnerable to fracture.1 Your doctor may recommend monitoring a benign tumor closely, including periodic X-rays or other tests to see whether the tumor changes.1
For malignant bone tumors, a team of doctors from multiple specialties will work with you to determine your treatment plan. Treatment depends on several factors. Malignant bone tumors are typically treated with a combination of chemotherapy, radiation and surgery.1 In general, more than 80% of patients with extremity osteosarcoma, a type of malignant bone tumor, can be treated by a limb-sparing procedure and do not require amputation.2
When surgery to salvage the limb is part of a treatment plan, bone may be replaced with an implant. If the tumor is in the femur (thigh) or tibia (shinbone), a doctor may consider an implant like Stryker’s Global Modular Replacement System (GMRS®) to replace the diseased bone.
LEARN MORE ABOUT STRYKER'S GLOBAL MODULAR REPLACEMENT SYSTEM® (GMRS)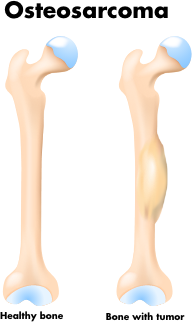
Types of sarcoma (malignant bone cancer)
A malignant bone tumor may be a primary bone cancer, which begins in bone, or a secondary bone cancer, which begins somewhere else in the body and then spreads to bone.1 According to the Academy of Orthopaedic Surgeons, the four most common types of primary bone cancer are multiple myeloma, osteosarcoma, Ewing sarcoma and chondrosarcoma.
Multiple myeloma1
Multiple myeloma is the most common primary bone cancer. It is a malignant tumor of bone marrow—the soft tissue in the center of many bones that produces blood cells. Any bone can be affected by this cancer. Multiple myeloma affects approximately seven people per 100,000 each year. According to the National Cancer Institute, more than 130,000 people are living with the disease each year. Most cases are seen in patients between the ages of 50 and 70.
Osteosarcoma1
Osteosarcoma is the second most common primary bone cancer. It occurs in two to five people per million each year, with most cases in teenagers and children. Most tumors develop around the knee in either the femur (thighbone) or tibia (shinbone). Other common locations include the hip and shoulder.
Ewing sarcoma1
Ewing sarcoma usually occurs in patients between the ages of 5 and 20. The most common locations affected are the upper and lower leg, pelvis, upper arm and ribs.
Chondrosarcoma1
Chondrosarcoma is a malignant
Chondrosarcoma is a malignant tumor composed of cartilage-producing cells. It is most often seen in patients between the ages of 40 and 70. Most cases occur around the hip, pelvis or shoulder area.
References:
- Rajani R, Quinn RH. Bone tumor. OrthoInfo. Accessed June 5, 2020. https://orthoinfo.aaos.org/en/diseases--conditions/bone-tumor/
- PDQ Pediatric Treatment Editorial Board. Osteosarcoma and Undifferentiated Pleomorphic Sarcoma of Bone Treatment (PDQ®): Health Professional Version. 2024 Dec 2. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002–. PMID: 26389179.
The Global Modular Replacement System (GMRS) is intended for use in patients requiring extensive reconstruction of the hip joint and/or knee joint, including knee fusions, necessitated by extensive bone loss due to trauma, failed previous prosthesis and or tumor resection.
GMRS is not appropriate for patients with:
- A condition that may have already resulted in either local or distant spread of a tumor such as pathological fracture, overt infection, inopportune placement of biopsy incision and rapid disease progression beyond a respectable margin.
- Certain types of infections or any mental or neuromuscular disorder which would create an unacceptable risk of prosthesis instability, prosthesis fixation failure, complication in postoperative care, compromised bone stock or inadequate bone stock.
- Skeletal immaturity.
As with any surgery, reconstruction of the hip joint and/or the knee joint has serious risks which include, but are not limited to, pain, infection, bone fracture, peripheral neuropathies (nerve damage), circulatory compromise (including deep vein thrombosis (blood clots in the legs)), genitourinary disorders (including kidney failure), gastrointestinal disorders (including paralytic ileus (loss of intestinal digestive movement)), vascular disorders including thrombus (blood clots), blood loss or changes in blood pressure or heart rhythm, bronchopulmonary disorders (including emboli, stroke or pneumonia), heart attack and death.
Implant-related risks which may lead to a revision include dislocation, subluxation, loosening, fracture, nerve palsy, subclinical nerve damage, soft tissue imbalance, osteolysis, intravascular extension of the tumor, metal sensitivity reactions and/or accelerated wear of the prosthetic implants. Global Modular Replacement System implants may not provide the same feel or performance characteristics experienced with a normal healthy joint.
The information presented is for educational purposes only. Speak to your doctor to decide if hip and/or knee reconstruction surgery is right for you. Individual results vary and not all patients will return to the same activity level. The lifetime of any joint replacement is limited and varies with each individual. Your doctor will counsel you about how to best maintain your activities in order to potentially prolong the lifetime of the device. Such strategies include not engaging in high-impact activities, such as running, as well as maintaining a healthy weight. It is important to closely follow your doctor’s instructions regarding post-surgery activity, treatment and follow-up care. Ask your doctor if a hip and/or knee joint reconstruction is right for you.
Stryker Corporation or its divisions or other corporate affiliated entities own, use or have applied for the following trademarks or service marks: GMRS, Stryker. All other trademarks are trademarks of their respective owners or holders.
JR-GMRS-PTNT-1530584